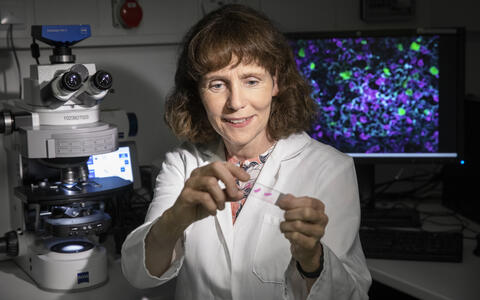
The trainer
The video shows a moment of destruction. Blue CAR T cells attack red dyed tumor cells, and light up at every encounter with their target. “This is evidence that they are releasing a substance to kill the tumor cells,” says Dr. Uta Höpken, pointing to her screen. Höpken, who heads the Microenvironmental Regulation in Autoimmunity and Cancer Lab at the Max Delbrück Center for Molecular Medicine (MDC), produced the combative immune cells with her team. She placed them in a cell culture with cancer cells and recorded how they reacted: After just 30 minutes, a single one of her CAR T cells had destroyed more than 15 tumor cells – leaving behind a trail of death and destruction in the surrounding tissue.
CAR T cells: The cancer killers
This clearly showed the potential that CAR T cells have. You can basically cure some cancers with such therapies.
CAR T cells are providing new hope for cancer patients, especially as a therapy for blood and lymph node cancers. They target unique features or antigens on the surface of tumor cells that can normally hide from the immune system. Scientists produce the cancer killing cells by genetically modifying T cells from patients’ blood to create a kind of antenna on their surface, so-called chimeric antigen receptors (CARs). These receptors rob the otherwise “invisible” tumor cells of their camouflage – and proceed to kill them one after another, as Höpken’s video shows.
The microscopic fighters are so successful that in 2018 the first CAR T-cell therapy was approved in Europe. It targets certain forms of B-cell leukemias and lymphomas. “This clearly showed the potential that CAR T cells have,” says Höpken. “You can basically cure some cancers with such therapies.” Together with her team, the researcher is searching for new antigens that could serve as targets for CAR T cells – and she is using this knowledge to produce the cancer killing cells in the lab and to train them to fight other forms of blood and lymph node cancers.
An amazing swarm of cells – with its own laws
Early on biology became Höpken’s favorite lens through which to see and understand the world. As a teenager, she read the books of primatologist Jane Goodall and dreamed of studying animals in Africa. But as a biology student, she realized that molecules excited her more – as did medical lectures on topics like immunology, virology, parasitology and microbiology. So she specialized in human biology, finding the immune system a worthwhile challenge to pursue. “Nothing about it is static; it’s an amazing swarm of T and B cells, macrophages and dendritic cells, constantly traveling and patrolling through the organs and blood vessels,” she says with her characteristic measured enthusiasm.
The topic of cell movement took hold of Höpken and never let her go. For her doctoral thesis, she observed how cells of the innate immune system migrate to the site of inflammation because they carry a receptor that responds to certain substances – ligands – which are released there. She went on to develop a monoclonal antibody that makes use of this receptor, and conducted studies on whether it can help treat sepsis. In 1994 she moved to Boston to attend Harvard Medical School.
“Chemokine receptors were first described while I was in the United States,” says Höpken. “They attract cells to the site of inflammation.” So did the receptor she was studying at the time. It was soon discovered that some chemokine receptors are required for HIV viruses to latch onto human immune cells before infecting them. This new class of receptors became known worldwide – and Höpken was right in the thick of things. On the other side of the Atlantic, Professor Martin Lipp, a cancer researcher at the MDC, came across a chemokine receptor that was unusual because it responded to a ligand that is released under normal conditions without inflammation.
Contract killers with a knack for detection
I was fascinated by how orderly everything was; nothing about it was arbitrary. You could see exactly where the B cells migrated to.
When she saw Lipp’s paper in Cell in December 1996, Höpken was blown away by the images of a mouse spleen that the team had made using three-color immunofluorescence staining: the T cells were colored blue and the B cells green and red. The images strikingly illustrated the important role of a single chemokine receptor called CXCR5 in cell movement: for example, how CXCR5 helps mature B cells to find their way from the bone marrow to their target – the B-cell zones in lymphoid organs like the lymph nodes and spleens – and to co-develop the internal structure of these organs. “I was fascinated by how orderly everything was; nothing about it was arbitrary. You could see exactly where the B cells migrated to,” recalls Höpken. Shortly thereafter she decided to join the MDC.
In Berlin, it wasn’t long before she was looking at tumor cells under the microscope. This research involved following where cancer cells migrate when they carry – or don’t carry – chemokine receptors like CCR7 and CXCR5 as navigational aids, leading her to discover that this receptor class plays a key role in tumor development. In recent years, she has increasingly been turning her attention to the niches in which tumor cells become lodged. This has required her to inventory the cell types in this microenvironment and study how cancer cells interact with healthy cells in order to employ them for their malignant purposes. “Tumor cells can alter scaffold cells and immune cells like macrophages, neutrophils and dendritic cells so that these cells no longer fight the cancer, but instead help tumor cells grow and multiply,” explains Höpken.
“I want to help cancer patients”
Around 2015, she felt she finally understood enough about tumor cell migration and the process of communication between tumor cells and their microenvironment – known as “crosstalk” – to develop therapeutic approaches using CAR-T cells, choosing to target blood cancer cells because they can recognize their receptors. “I was motivated by a deep need to help cancer patients,” says Höpken. Two of her “contract killers” have since proved effective: one against multiple myeloma, a bone marrow cancer, and the second against certain blood and lymph node cancers like follicular lymphoma and chronic lymphocytic leukemia. “If all goes according to plan, we will be able to treat the first patients in 2022,” says Höpken.
Some questions still need to be answered before these CAR T cells can be approved for therapy in patients. That’s because although CAR T cells target cancer antigens, they also kill “normal” B cells and can inadvertently attack other molecules. Experiments in mice have shown that CAR T cells directed against CXCR5 reliably eliminate tumor cells – and that the animals did not suffer from the loss of their healthy B cells. The research also showed that the CAR T cells did not damage liver, kidney and glial cells. However, clinical trials in humans must determine how well the therapy actually works.
Delivering new therapies to cancer patients faster
You can detect a note of impatience in Höpken’s voice when she talks about therapeutic development and approval. She believes that many things move too slowly, that some things are overregulated, and that it’s virtually impossible to describe the extent of the bureaucracy to terminally ill patients. To speed up the process, she is actively supporting the National Center for Tumor Diseases (NCT), which is establishing a site on the Virchow Campus in Berlin’s Wedding district. “Patients will have access to the latest therapies at the new site as well as educational resources that allow them to expand their knowledge and better understand cancer studies,” says Höpken. Patient representatives will have a say in therapeutic development at the NCT. “This step is absolutely necessary to bring promising therapies to patients faster.”
I was fascinated by how orderly everything was; nothing about it was arbitrary. You could see exactly where the B cells migrated to.
Höpken could have switched to the pharmaceutical industry long ago. But having intellectual freedom is much more important to her than regular working hours with triple the salary. She also enjoys being able to work closely with young people at the research center and train doctoral students. “I can decide on which type of cancer I want to develop a CAR T cell for on the weekend and get started with it on Monday,” she says. In fact, her Sundays are not set aside for rest and relaxation; she doesn’t believe in separating work and leisure. “For me, both are an integral part of life,” she says. “On Sundays I like to keep busy with things I want to start in the coming week.” Only her Sunday morning run in the woods is sacred.
As for her work at the MDC, Höpken hopes to be able to engineer a new set of CAR T cells that are capable of fighting other cancers, not just leukemias and lymphomas. For example, together with Dr. Annette Künkele of Charité – Universitätsmedizin Berlin, she has set her sights on neuroblastoma, a cancer that attaches itself to the spine or adrenal gland and primarily affects children. She wants to help influence the tumor microenvironment in a way that makes CAR T cells work more effectively. “The world will never be cancer-free. But we must try to transform as many cancers as possible from lethal to chronic diseases,” says Höpken. “And maybe we’ll succeed in curing some of them.”
Text: Mirco Lomoth